RCTX CE Event: Cases Referred By You
On May 24, 2022, Retina Consultants of Texas presented its first virtual zoom CE event of the year on some interesting cases that have been referred to our doctors in Houston and San Antonio over the past couple of years. Hosted by Dr. James Major, the webinar consisted of three sections presented by Dr. William Pearce, Dr. Vy Nguyen, and Dr. Moises Chica, with Dr. Rosa Kim, Dr. Sarah Holy, Dr. Matthew Benz, Dr. Tien Wong, Dr. R. Gary Lane, and Dr. Christopher Henry providing additional commentary, questions, and discussion.
Presentation #1: Dr. Pearce
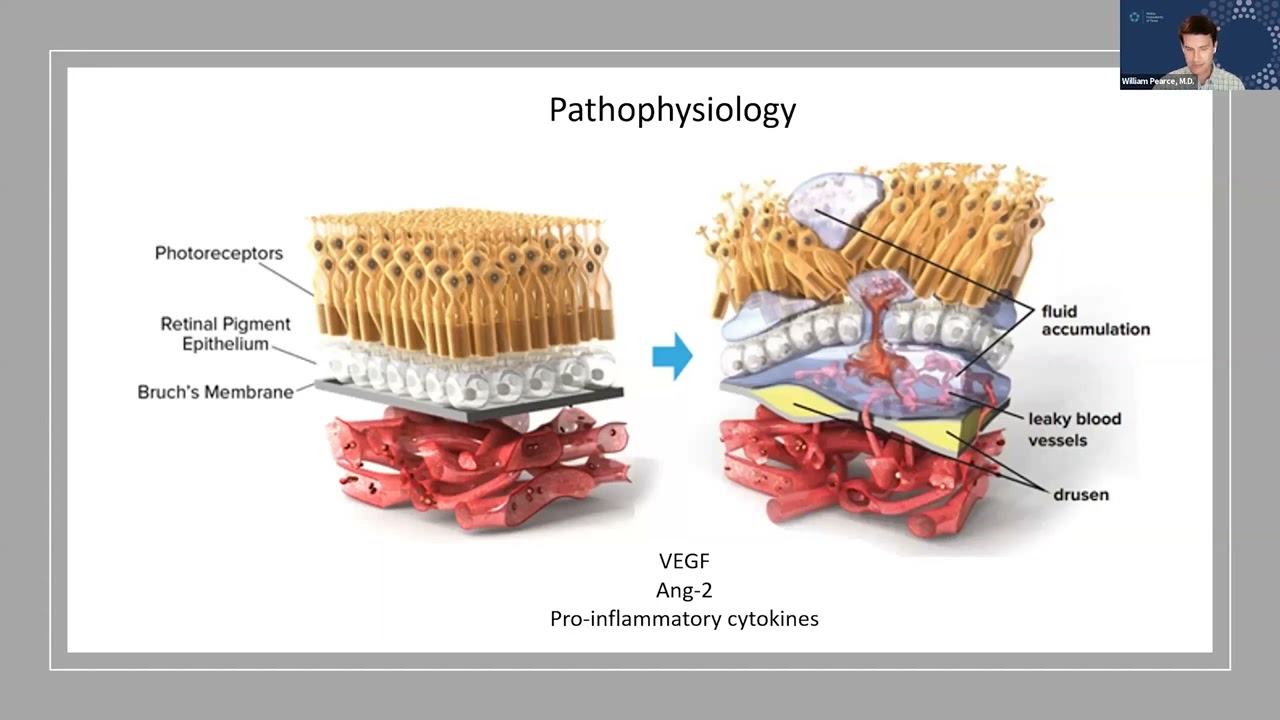
Dr. Pearce's presentation focused on a “bread and butter” case of neovascular age-related macular degeneration (also referred to as wet AMD). The case was a 75-year-old woman who had central distortions in her right eye’s field of vision, which she discovered by using an Amsler grid at home. Dr. Pearce used a wide range of optical coherence tomography (OCT) images of the patient’s eye to explain his diagnostic process and the type of signs he’s looking for when looking at an image, touching on subtopics such as the retinal vasculature, hemorrhaging, edemas, posterior vitreous detachment (PVD), intra-retinal and sub-retinal fluid, retinal contouring, and tissue atrophy.
He went on to discuss possible differential diagnoses, preventive measures, and treatment options. The panel discussed the usage of Eylea injections for wet AMD, as well as the possibility of finding eligible clinical trials. Dr. Pearce’s presentation concluded with an overview of current and future treatment modalities for wet AMD, citing anti-vegetative endothelial growth factor (anti-VEGF) injections as the workhorses of retinal care and talking a little bit about the recent development of the port delivery system. He also talked a little bit about the future of gene therapy in retinal care, explaining how the idea behind gene therapy will be to teach the retina to produce its own anti-VEGFs.
Presentation #2: Dr. Vy Nguyen
Dr. Nguyen’s presentation focused on two distinct cases that both ended up being branch retinal artery occlusion (BRAO). Using extensive imaging, Dr. Ngyuen revealed telltale signs of BRAO in both cases. The first case was an 86-year-old man who reported experiencing a shadow or curtain of darkness over his vision. Fundus photography revealed scattered areas of whitening, as well as a chorioretinal scar. Further investigation showed that both eyes had a partial PVD and retinal thickening. Based on these findings, Dr. Ngyuen performed a fluorescein angiogram, which revealed a lot about the patient’s ocular vasculature. She started a workup immediately for BRAO and referred him to a stroke center, as patients who experience occlusive events in their eyes have an increased risk of experiencing a cerebral stroke.
Dr. Ngyuen then presented a second case featuring a female patient in her 60s presenting with an inferior defect in her visual field. Dr. Ngyuen’s diagnostic imaging scans found acute thickening and injury to the inner retina. An angiogram revealed that the patient had a blocked retinal artery. Using these two cases, Dr. Ngyuen discussed various aspects of BRAO, including risk factors, clinical presentations, treatments, and complications with a special focus on neovascularization issues.
Presentation #3: Dr. Moises Chica
Dr. Chica explored retinal vein occlusions using three distinct cases of patients he had treated over the years. He touched on several important points, including how:
- Retinal vein occlusion is the most common retinal vascular disorder after diabetic retinopathy
- Retinal ischemia can increase the eye’s VEGF load, turning normal blood vessels into overactive “soakers”
- Branch retinal vein occlusion (BRVO) is more common than central retinal vein occlusion (CRVO)
- Retinal vein occlusions can lead to macular edema, neovascularization, vitreous hemorrhage, and, in some cases, tractional retinal detachment
- If ischemia occurs in the fovea, it is untreatable
After presenting each case, Dr. Chica opened up the discussion to the panelists. Together, they discussed how soon a patient with retinal vein occlusion should be treated, as well as how catastrophic it can be to have gaps in treatment, especially in comparison to treating diseases like AMD.
Referring to Retina Consultants of Texas
As the leading retina-only ophthalmology practice in Texas, we work with thousands of referring physicians throughout Houston, San Antonio, and beyond. Learn more about how to refer a patient to our practice or fill out a patient referral form. We have a physician on call 24/7, including weekends and holidays.
We invite you to watch the full video of our “Cases Referred By You: Diagnosis and Management of Retinal Conditions” presentation on our YouTube channel. To attend Retina Consultants of Texas’s next CE Zoom event, please register here for updates.